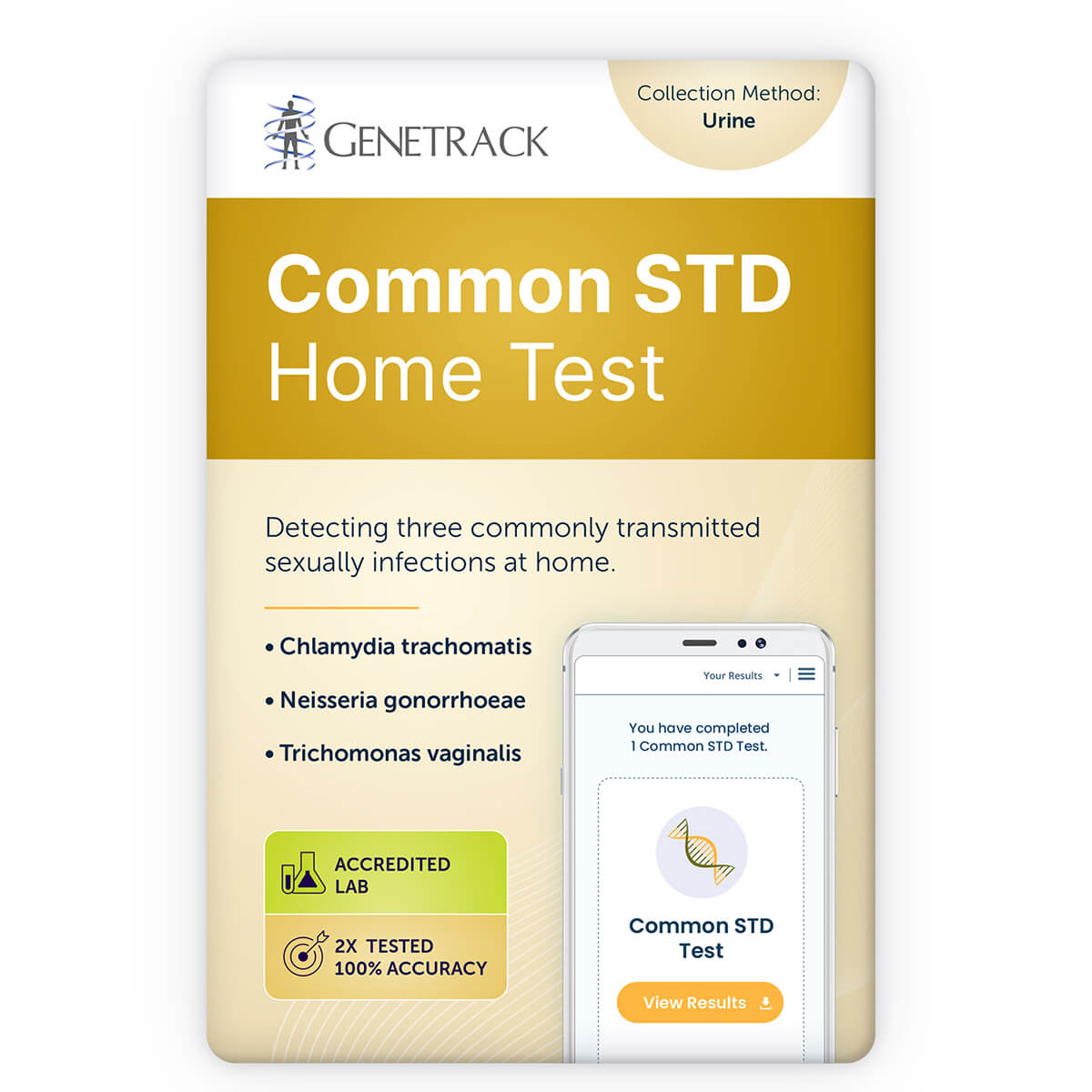
Common STD Test
Chlamydia, gonorrhea and trichomoniasis are common sexually transmitted diseases (STDs) caused by Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis. Both men and women can be infected; however, many infected individuals do not show any symptoms. Early detection enables prompt treatment to prevent transmission and long-term health complications, such as pelvic inflammatory disease and infertility.
$99.00
Details
What is Included?
Detection of Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis by nucleic acid amplification technology
Turnaround Time
1 – 3 business days
The turnaround time is not guaranteed. The average turnaround time is 1 – 3 business days from the date that the sample arrives at the laboratory. Shipping time for the sample is not included. Additional time is required if the case requires confirmatory or reflex testing, or if the sample is insufficient, or if a recollection is required.
Related Documents
- Patient Brochure
- Physician Brochure
- Sample Report
Additional Information and Resources
SPECIMEN REQUIREMENTS
Preparation Before Specimen Collection
- Do not urinate for at least one hour prior to urine collection.
- Females should not cleanse the labial area prior to urine collection.
- Antibiotics can affect this test so wait until at least seven days after completing a course of antibiotics before collecting your urine sample.
- This test may need to be repeated to ensure the accuracy of any negative results that are obtained from samples collecting within the window period post-exposure (approximately two weeks for chlamydia and gonorrhea, and 3–6 weeks for trichomoniasis).
Specimen Type
First-void urine
Urine sample collected from the initial urine stream at least one hour after previous urination.
Volume
2 mL from a 20 – 30 mL collection of first-void urine.
Repeat urine collection (at least 1 hour after previous urination) if more than 60ml of first-void urine is collected.
Container
Urine specimen transport container
Collection Method
This test requires a first-void urine specimen. Wait at least 1 hour after previous urination before collecting the first-void urine. All supplies for sample collection are provided in this kit.
- Collect 20 – 30 mL from the initial urine stream into the sterile urine collection container. Collection of larger volumes of urine may result in specimen dilution that may reduce test sensitivity; lesser volumes may not adequately rinse organisms into the specimen.
- Transfer 2 mL of urine into the urine specimen transport container using the disposable pipette provided. Transfer to the urine specimen transport container must occur within 24 hours of collection, and liquid level must fall between the two black indicator lines on the tube label.
- Re-cap the urine specimen transport container tightly. Seal in the transport bag and return to the laboratory in the provided prepaid return-shipping envelope.
Specimen Storage
Maintain specimen at temperatures between 2°C and 30°C during storage and transport.
Specimen Stability
Specimens stored at temperatures between 2°C and 30°C must be tested within 30 days of collection. If longer storage is required, urine specimens may be frozen in the urine specimen transport container within 7 days of collection and tested within 12 month of collection.
Causes for Rejection
- Incorrect or incomplete patient identification
- Incorrect specimen collection
- Inappropriate storage and transport conditions
- Loss of urine specimen through container leakage
- Incorrect specimen volume
- Specimen received >30 days after collection
TEST DETAILS
Purpose
To detect Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis nucleic acid in a urine specimen
Limitations
- This report is not intended for use in medico-legal applications.
- These results are intended for screening and monitoring for chlamydia, gonorrhea, and trichomoniasis and should be interpreted in conjunction with other laboratory and clinical information.
- Correct specimen collection and handling is required for optimal assay performance.
- The effects of tampon use, douching, and specimen collection variables have not been assessed for their impact on the detection of chlamydia, gonorrhea, and trichomoniasis.
- A negative result does not exclude the possibility of infection. False-negative test results may occur due to improper specimen collection, concurrent antibiotic therapy, presence of inhibitors, or organism levels below the sensitivity of this assay (which is common within 2 weeks post-exposure for chlamydia and gonorrhea, and within 3-6 weeks for trichomoniasis).
- False-positive results are rare, but may be more frequent in low-prevalence populations. A false-positive result may also occur directly after successful antimicrobial therapy, as Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis nucleic acids may persist for 3 weeks or more. For this reason, this test cannot be used for determining therapeutic success or failure.
- The performance of this assay has not been evaluated in adolescents less than 14 years of age.
- Female urine specimens may detect up to 10% fewer infections when compared with vaginal and endocervical swab specimens.
Methodology
Nucleic acid amplification