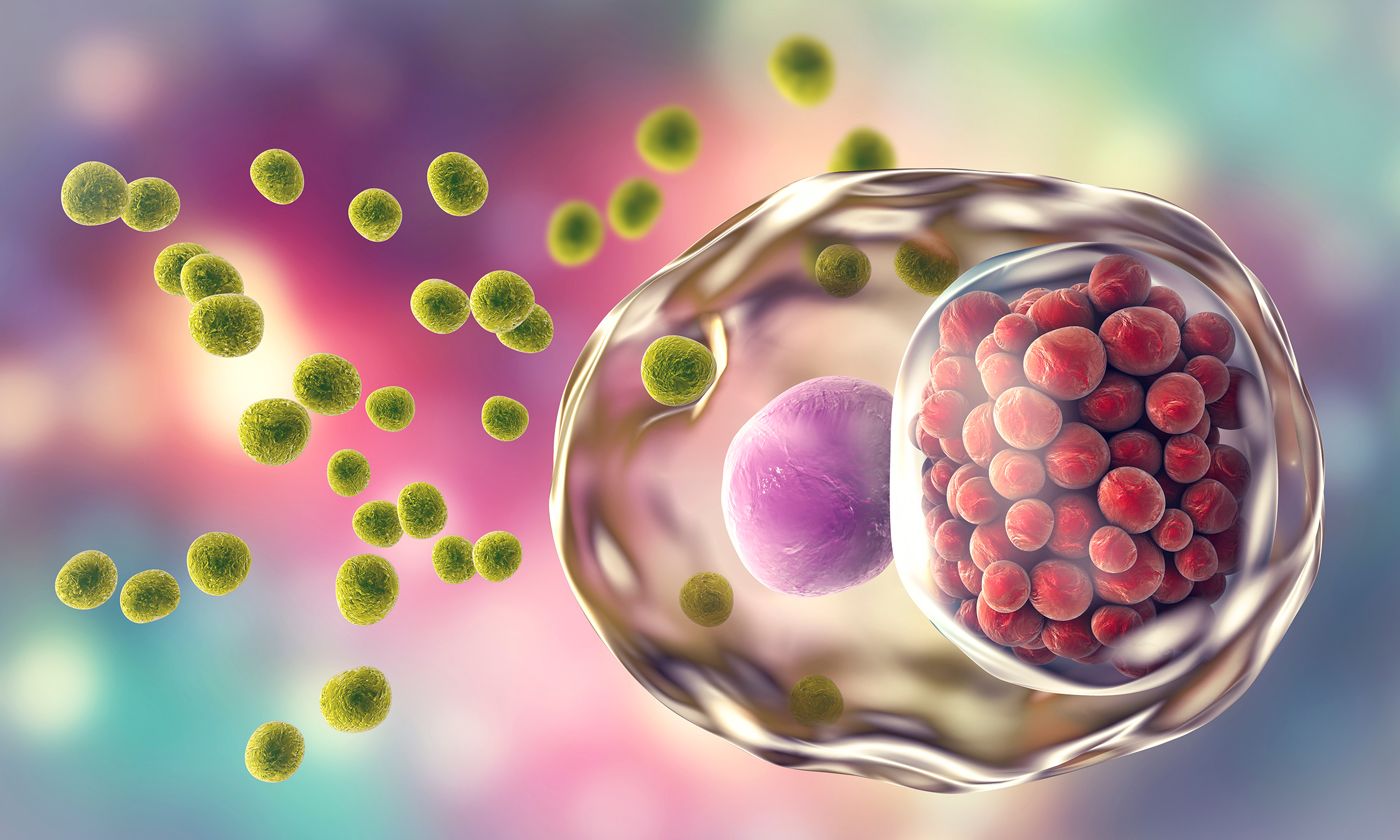
Chlamydia is a common sexually transmitted disease (STD) caused by infection with the obligate intracellular bacterium Chlamydia trachomatis. Chlamydia is transmitted through sexual contact with the penis, vagina, mouth, or anus of an infected individual. It can also be transmitted from a mother with an untreated chlamydial cervical infection to her newborn during childbirth (1).
Chlamydia can cause abnormal vaginal discharge, endocervical bleeding, increased urinary frequency, and dysuria in females, and urethral discharge, dysuria, and testicular pain in males. Chlamydia infections of the rectum may lead to proctitis, rectal pain, discharge and/or bleeding (2). Sexually acquired chlamydial conjunctivitis can also occur in both males and females (3). However, most individuals infected with chlamydia remain asymptomatic, with only an estimated 10% of infected males showing symptoms and 5-30% of infected females (4; 5).
Despite the absence of disease symptoms in many individuals, long-term health complications can still occur. Complications in females include pelvic inflammatory disease (PID), infertility, ectopic pregnancy, preterm delivery, and increased risk of disease in newborns. Complications in untreated males are rare, but can include epididymitis and infertility. Chlamydial infections can also facilitate the transmission of HIV infection (6), and in rare cases can cause reactive arthritis (7).
Pelvic Inflammatory Disease (PID)
PID is an infection of a female’s reproductive organs. It is often caused by an untreated STD infection, such as chlamydia, which moves upwards from the vagina/cervix into the reproductive organs. The proportion of females with untreated chlamydia that develop PID varies significantly between studies, but is estimated to be around 16% (8; 9). Other microorganisms have also been implicated in the pathogenesis of PID (10).
Some individuals do not experience any symptoms or only show mild symptoms. Symptoms can include lower abdomen pain, fever, abnormal vaginal discharge with an unpleasant odor, pain and/or bleeding during sexual intercourse, painful and frequent urination, and bleeding between periods (11).
PID is usually diagnosed based on medical history, physical exams, and other test results. Pelvic examinations are used to detect cervical motion, uterine, and/or adnexal tenderness. Inflammation in the lower genital tract can be detected by a predominance of leukocytes (white blood cells) in vaginal secretions, elevated C-reactive protein, and cervical friability (sensitive and irritated cervix tissue). Additional diagnostic tools include endometrial biopsy, transvaginal sonography and MRI (12).
Treatment of PID is with broad-spectrum antibiotics to cover likely pathogens. However, antibiotics do not heal any tissue damage already caused by PID. It is important for any prescribed medications to be taken properly and completely, and any sexual partners should be treated concurrently (12).
Infertility in Females
Untreated PID is associated with an increased risk of infertility, particularly in females with recurrent episodes of PID and severe tubal inflammation (11). However, infertility can also occur in individuals with subclinical PID (13); hence why prompt diagnosis and treatment of chlamydia is very important.
Ectopic Pregnancy
Inflammation associated with chlamydia increases the risk of ectopic pregnancy, which is when the fertilized egg implants and grows outside the main cavity of the uterus (14). An ectopic pregnancy cannot proceed as normal and may cause life-threatening bleeding if untreated. Early symptoms can include light vaginal bleeding, pelvic pain, and an urge to have a bowel movement. If the fallopian tube ruptures, heavy internal bleeding occurs causing fainting and shock (14).
Preterm Delivery
Chlamydial infections during pregnancy are associated with preterm delivery with studies reporting a 4-fold increased risk for delivery before 32 weeks gestation (15), and 2- to 3-fold increased risk for delivery before 35 weeks (15; 16). Premature births increase the risk of several complications, including problems associated with breathing, the heart and brain, temperature control, digestion and metabolism. Long-term complications of a premature birth can include cerebral palsy, impaired learning, vision and hearing problems and chronic health issues.
Disease in Newborns
Untreated chlamydia during pregnancy is associated with a 50-70% risk of passing the infection to the newborn during childbirth. This increases the risk of conjunctivitis (18-44% of cases) and pneumonia (3-16% of cases) (17; 18; 19). Untreated conjunctivitis may last for months and cause corneal and conjunctival scarring (19). Pneumonia is the leading cause of death in the neonatal period (20).
Epididymitis
Epididymitis is a clinical syndrome most frequently caused by chlamydial or gonorrheal infections. It is characterized by pain, swelling, and inflammation of the epididymis, and sometimes the testis (known as epididymo-orchitis). Treatment is by antibiotic therapy to cure the underlying infection. Sexual partners should also undergo treatment to prevent reinfection after the treatment course (21).
Infertility in Males
Chlamydial infections in males are associated with dramatic genetic changes in sperm, which reduce male fertility. However, standard antibiotic treatment for chlamydia significantly improves fertility again in affected males (22).
HIV
Chlamydial infections increase the risk of getting HIV, due to the presence of chlamydial-associated inflammation and sores (6). Chlamydia in HIV-positive individuals also increases the risk of passing HIV to any sexual partners, although effective HIV-treatment prevents this risk.
Reactive Arthritis
Reactive arthritis (aka Reiter’s syndrome) is joint inflammation that develops as a reaction to an infection in another area of the body. Chlamydia is the most common cause of reactive arthritis in the United States (23).
References:
1. Sexually Transmitted Disease Surveillance, 2018. CDC. October 2019.
2. Thompson CI, MacAulay AJ, Smith IW. (1989). Chlamydia trachomatis infections in the female rectums. Genitourin Med, 65 (4), 269-273.
3. Kalayoglu MV. (2002). Ocular chlamydial infections: pathogenesis and emerging treatment strategies. Curr Drug Targets Infect Disord, 2 (1), 85-91.
4. Farley TA, Cohen DA, Elkins W. (2003). Asymptomatic sexually transmitted diseases: the case for screening. Prev Med, 36 (4), 502-509.
5. Korenromp EL, et al. (2002). What proportion of episodes of gonorrhoea and chlamydia becomes symptomatic? Int J STD AIDS, 13 (2), 91-101.
6. Fleming DT and Wasserheit JN. (1999). From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect, 75 (1), 3-17.
7. Cheeti A, Chakraborty RK, Ramphul K. (2020) Reactive Arthritis (Reiter Syndrome). StatPearls (Internet). Treasure Island : StatPearls Publishing, 2020, Vol. January.
8. Price MJ, et al. (2013). Risk of Pelvic Inflammatory Disease Following Chlamydia trachomatis Infection: Analysis of Prospective Studies With a Multistate Model. Am J Epidemiol, 178 (3), 484-492.
9. Reekie J, et al. (2018). Risk of Pelvic Inflammatory Disease in Relation to Chlamydia and Gonorrhea Testing, Repeat Testing, and Positivity: A Population-Based Cohort Study. Clin Infect Dis, 66 (3), 437-443.
10. Hillier SL, et al. (1996). Role of bacterial vaginosis-associated microorganisms in endometritis. Am J Obstet Gynecol, 175 (2), 435-441.
11. Pelvic Inflammatory Disease (PID) Detailed Fact Sheet. CDC. January 2017.
12. Workowski KA and Bolan GA. (2015). Sexually Transmitted Diseases Treatment Guidelines, 2015. MMWR. 64 (RR3), 1-137.
13. Wiesenfeld HC, et al. (2012). Subclinical pelvic inflammatory disease and infertility. Obstet Gynecol, 120 (1), 37-43.
14. Murray H, et al. (2005). Diagnosis and treatment of ectopic pregnancy. CMAJ, 173 (8), 905-912.
15. Rours GI, et al. (2011). Chlamydia trachomatis infection during pregnancy associated with preterm delivery: a population-based prospective cohort study. Eur J Epidemiol, 26 (6), 493-502.
16. Andrews WW, et al. (2000). The Preterm Prediction Study: association of second-trimester genitourinary chlamydia infection with subsequent spontaneous preterm birth. Am J Obstet Gynecol, 183 (3), 662-668.
17. Hammerschlag MR, et al. (1982). Longitudinal studies of chlamydial infection in the first year of life. Pediatr Infect Dis, 1 (6), 395-401.
18. Heggie AD, et al. (1981). Chlamydia trachomatis infection in mothers and infants: A prospective study. Am J Dis Child, 135 (6), 507-511.
19. Chlamydia of the Newborn. Pediatrics Clerkship, The University of Chicago.
20. Mishra KN, et al. (2011), Acute Chlamydia trachomatis Respiratory Infection in Infants. J Glob Infect Dis, 3 (3), 216-220.
21. 2015 Sexually Transmitted Diseases Treatment Guidelines, Epididymitis. CDC. June 2015.
22. Gallegos G, et al. (2008). Sperm DNA fragmentation in infertile men with genitourinary infection by Chlamydia trachomatis and Mycoplasma. Fertility and Sterility. 90 (2), 328-334.
23. Carter. Reactive Arthritis. Rare Disease Database.