Firstly, let’s go over a few quick facts about gonorrhea:
- It is a common sexually transmitted disease (STD) or sexually transmitted infection (STI).
- It is spread through sexual contact with the penis, vagina, mouth, or anus of an infected individual.
- It can also spread from a mother to her newborn during childbirth.
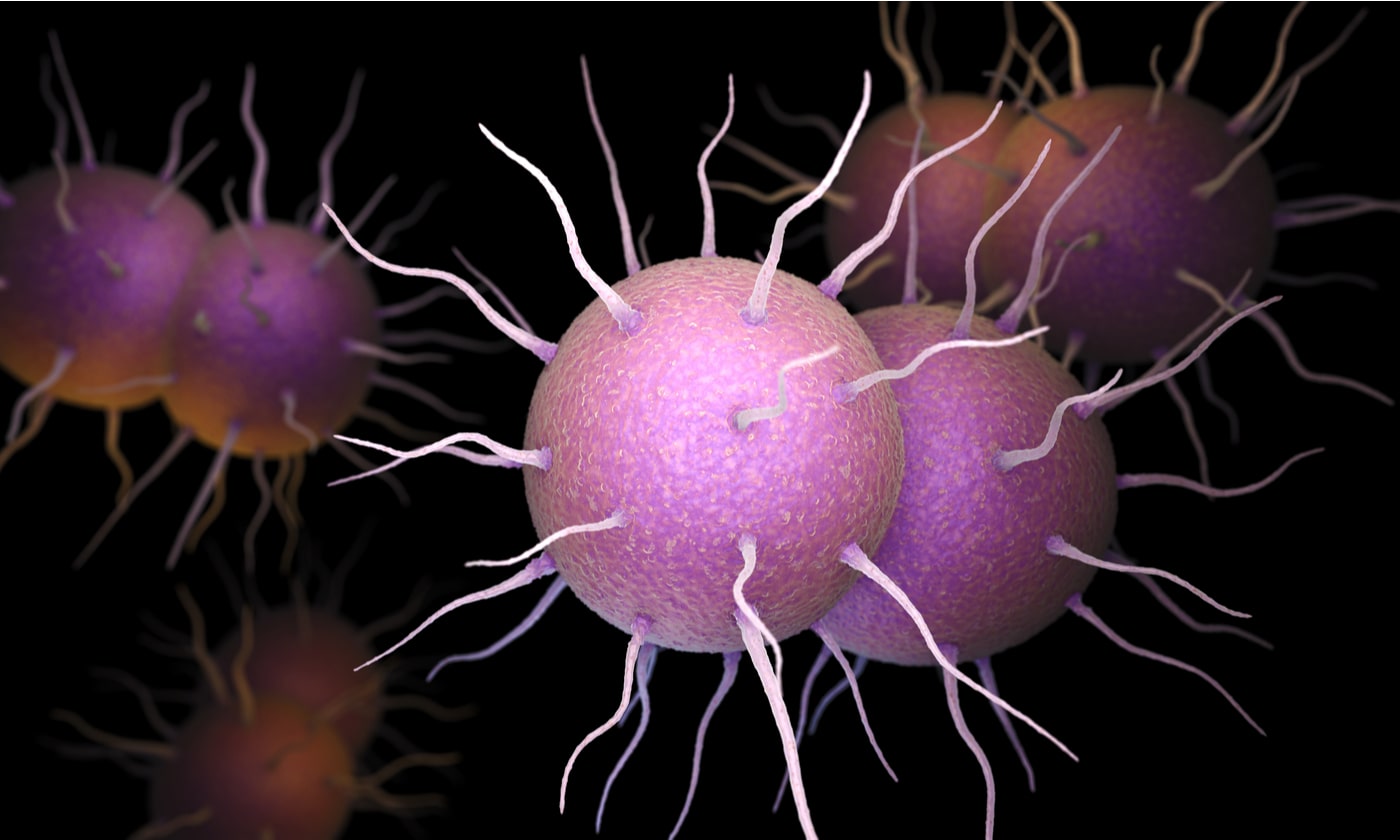
- It is caused by infection with the bacterium Neisseria gonorrhoeae.
- 85–90% of males show symptoms of a urogenital infection but only <20% of females. Urogenital refers to the urinary tract, vagina, or penis.
How does oral gonorrhea occur?
Oral gonorrhea is also known as pharyngeal gonorrhea. It refers to a gonorrhea infection in the throat and can occur by giving oral sex to a partner with an infected penis, urinary tract, vagina, or rectum (1). Basically, the Neisseria gonorrhoeae bacterium isn’t too fussy about which mucus membranes it infects, so it is quite happy to spread to the mucus membranes in the throat. Gonorrhea transmission can occur even when an infected person is not showing any symptoms.
What are the symptoms of oral gonorrhea?
Most people with an oral gonorrhea infection do not experience any symptoms. And if they do, it is going to feel like any other sore throat (1). Other symptoms can include redness in the throat, throat inflammation, and swollen glands (2).
Can untreated oral gonorrhea cause any serious complications?
Despite an often absence of symptoms from oral gonorrhea (or urogenital gonorrhea for that matter), serious health complications are rare but possible. The gonorrhea infection can spread throughout the body causing a condition called disseminated gonococcal infection (1). The symptoms can include fever, joint pain and swelling, and skin lesions. The joints that are most commonly affected are wrists, ankles, hands, and feet. In rare cases, the infection can also affect the liver, brain, and heart tissue (2). Disseminated gonococcal infection can be caused by both untreated oral gonorrhea and untreated urogenital gonorrhea (3).
How to test for oral gonorrhea?
Oral gonorrhea can be detected by culture and nucleic acid amplification tests (NAATs) of pharyngeal (throat) swabs (4).
At least annual screening for oral gonorrhea is recommended for men who have sex with men (MSM), with increased screening (every 3–6 months) for MSM at high risk (e.g., substance abuse or multiple partners) or those at high risk of HIV acquisition (4).
How is oral gonorrhea treated?
Increased antibiotic resistance previously raised concerns about gonorrhea treatment and dual antibiotic therapy was recommended. However, due to other health concerns, only ceftriaxone is now recommended by the CDC. This is administered via a shot in the muscle (4).
References:
1. STD Risk and Oral Sex, Sexually Transmitted Diseases (STDs). Reviewed Feb 2020. CDC.
2. Mayor MT, Roett MA, Uduhiri KA. (2012). Diagnosis and Management of Gonococcal Infections. Am Fam Physician, 86(10):931-938.
3. Morris SR. (2020). Gonorrhea. Merck Manual Professional Version.
4. Gonococcal Infections Among Adolescents and Adults. Sexually Transmitted Infections Treatment Guidelines, 2021. (Reviewed July 2021). CDC.